The Robotic HeartNathan Edelman
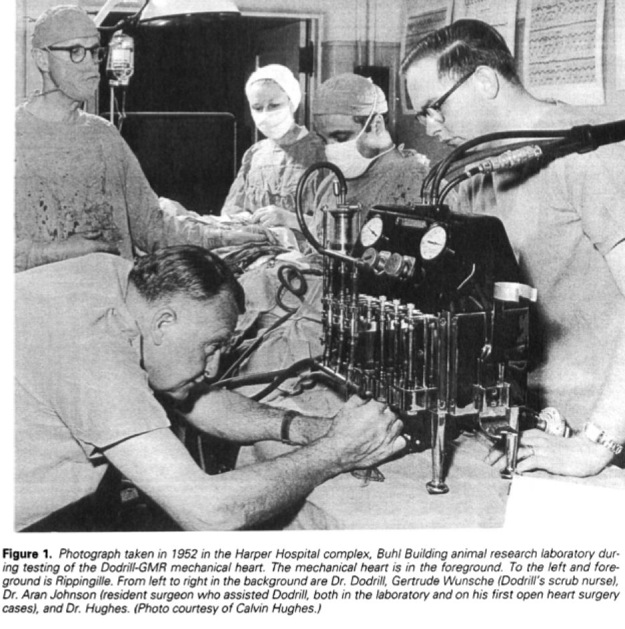
Scientific advancements in the area of mechanical body parts have created the reality that a hybrid human-robot, a cyborg, is no longer only a topic for science fiction. Extensive progress has been made in the area of mechanical body parts in the fields of all major organs, including bone, hemoglobin, legs and arms. Much progress has been made relating to brain implants, which are beneficial to patients with nervous system conditions, and the visually or audibly impaired. While clinical trials thus far have only focused on implanting one mechanical organ in a human, it is hypothetically possible that in the future one could have many of their organs replaced and become a living human robot, a cyborg. The heart specifically has been an area of intense research in the past fifty years. As seemingly simple a job the human heart has, humanity has never been able to fully replicate its function using mechanical components. The basic function of the heart is simple; pump blood to the cells of the body. The heart pumps blood every minute of every day, never needing to rest, slowing and speeding up as requested. With all the effort and knowledge of some of the world's most brilliant individuals, it appears possible that within the twenty-first century, a mechanical alternative to the human heart will be available. The Mechanical Heart: A Brief HistoryOn July 3, 1952, a 41-year-old male suffering from shortness of breath made medical history at Harper University Hospital in Michigan. The Dodrill-GMR heart machine, considered by some to be the first operational mechanical heart was successfully used while performing heart surgery (Stephenson, Arbulu and Bassett) (American Heart Association). The machine performs the functions of the heart, allowing doctors to detour blood and stop the heart of a patient during an operation. The machine is external of the body and is only used during an operation. Dr. Forest Dewey Dodrill, a surgeon at Wayne State University's Harper Hospital in Detroit, developed the machine with funding from The American Heart Association and volunteer engineers from General Motors (American Heart Association). Dr. Dodrill used the machine in 1952 to bypass Henry Opitek's left ventricle for 50 minutes while he opened the patient's left atrium and worked to repair the mitral valve. In Dodrill's post operative report he notes, “To our knowledge, this is the first instance of survival of a patient when a mechanical heart mechanism was used to take over the complete body function of maintaining the blood supply of the body while the heart was open and operated on (Stephenson, Arbulu and Bassett).” The machine has been improved greatly in the years since its first use and derivatives of the machine are very much in use today. Nearly a million open-heart procedures are performed each year. Impressive as this is, even more amazing is the development of a mechanical heart small enough to be installed inside the body, independently powered and a substitution for the natural human heart. A perfect substitute for the biological human heart probably won't be ready for decades, but significant progress has been made over the years. The Jarvik-7 is the first artificial heart implanted in a living being. It was placed in a dog at the Cleveland Clinic in 1957; it survived about 90 minutes (Sandeep Jauhar). In April of 1969, Denton Cooley, a surgeon at the Texas Heart Institute in Houston, used an artificial heart as a temporary bridge to transplantation in 47-year-old Haskell Karp (PBS). By some accounts the procedure was considered a success because Mr. Karp regained organ function. However, nobody will dispute the experience he had; A terrible quality of life. In an interview for PBS's Nova, His wife Shirley describes her husband in the days immediately following the operation: I saw apparatuses going into the arms, the hands, the feet. He could not say anything. I don't think that he was really conscious. One day they removed the tube from his throat, they put a sheet over all the apparatuses in back of him, and had the media take their pictures, saying, ‘look how well he's doing.' And immediately after this was done, they put back the resuscitation tube, and opened up everything that they had closed up. Mr. Karp succumbed to an infection three days later following the implantation of a biological heart from a donor. Ironically he might have lived longer if doctors never removed the mechanical heart (PBS) because he likely would not have contracted the infection. The next seven attempts at implantation of an artificial heart were unsuccessful and the public lost interest in the idea of a mechanical heart. Nearly twenty years would pass before the next documented attempt (Sandeep Jauhar). In 1982, Dr. William DeVries of the University of Utah implanted a dentist named Barney Clark with an artificial heart called the Jarvik-7. As a dentist, he felt he was helping science. Clark was 61 years old and suffering from end-stage congestive heart failure. Since Clark was too sick to be eligible for a donated heart, Clark's implant would be permanent. His condition as documented before the operation describes a man in extremely poor health: For months, he had had virtually intolerable shortness of breath, nausea, and fatigue. On Thanksgiving Day, family members had to carry him to the dinner table at his home in Seattle, but he was unable to eat. In the intensive care unit in Salt Lake City, he was placed in a dark room, and visitation was restricted because doctors feared that any sort of excitement could precipitate a life-threatening arrhythmia [A condition in which the heart beats with an irregular rhythm.]…death appeared imminent within hours to days (Sandeep Jauhar). “In the early morning of December 2 [1982], Clark came out of the operating room with plastic tubes coming out of his chest, connected to a refrigerator-sized machine. Though he was very much alive, his electrocardiogram was a flat line (Sandeep Jauhar).” Mr. Clark's condition after receiving the new heart was rather unpleasant: Although he opened his eyes and moved his limbs three hours after the operation, his subsequent course was rocky. On day 3, he underwent thoracic exploratory surgery because of subcutaneous emphysema. On day 6, he had generalized seizures that left him in a postictal coma. On day 13, his prosthetic mitral valve malfunctioned, and he had to go back to the operating room to have the left ventricle replaced. Many complications followed, including respiratory failure requiring a tracheostomy, renal failure, rampant fevers, aspiration pneumonia, pseudomembranous colitis, and sepsis. On day 92, DeVries spoke with Clark in a videotaped interview. ‘It's been hard, hasn't it, Barney?' DeVries said. ‘Yes, it's been hard,' Clark replied. ‘But the heart itself is pumping right along.' It continued to pump until he finally succumbed to multiorgan failure on day 112 (Sandeep Jauhar). On July 2, 2001, the first fully contained artificial heart, the AbioCor, from a company called Abiomed, was implanted in a 58-year-old man at Jewish Hospital in Louisville, Kentucky. The patient died five months later from a stroke (Sandeep Jauhar). The Ventricular Assist Device While research continues on developing new pumps and improving the current technology, much focus has also been centered on developing smaller pumps that complement rather than substitute the human heart. Instead of removing the human heart a lot of research is focusing on ventricular assist devices that can be implanted inside a patient and attached directly to a human heart as a prosthesis. One such ventricular assist device (VAD), the Kantrowitz CardioVad, Additionally, the VAD can help patients on the wait-list for a heart transplant. In a young person, this device could delay the need for a transplant by 10-15 years (Mitka). Congestive heart failure (CHF) affects about 1% of adults in the United States annually and is a contributing factor in about 250,000 deaths each year. CHF is diagnosed in about 400,00 Americans and is the primary diagnosis for over 900,000 hospitalizations every year (Goldstein, Oz and Rose). These numbers are only getting larger! The median survival after diagnosis is 1.7 years in men and 3.2 years in women (Goldstein, Oz and Rose). The five-year survival rate is less than 50%. The number of donor hearts available annually is chilling; 2,500 (Kenneth and Jarcho) (Goldstein, Oz and Rose)! People suffer and many die waiting for a heart to become available. The Ethics and Morals Perhaps one of the greatest ethical challenges facing the medical field today is allocating healthy organs to patients who need them most. Typically, in situations of scarcity, those who are willing and able to pay the prevailing market price for a good or service will receive the item. The market price is determined by economic forces within a market and not by any single individual. Via the price-system, society arrives at an incredibly efficient allocation of scarce resources. We as a society feel that when it comes to allocating life saving organs, it will create a gross imbalance of equity if allocation is based on ones ability to pay. Above, I mention that a person must be “willing and able” to pay the market price. It is the second word which is of most concern. Organ allocation is currently based on a wait list. Patients are prioritized based on need, possibility of survival after implantation and a number of other criteria. The unfortunate side effect is of course that demand far outpaces supply. Many people die each year waiting for an organ to become available. Mechanical organs can be manufactured. That is one major advantage they have over the extremely scarce biological organs. If X number of patients are in need, X number of organs can be manufactured to meet that need. Therefore there is no need to maintain a wait list. There should be no shortage of mechanical organs. Of course, it is still extremely costly to manufacture mechanical organs. The total cost of the transplant is extremely expensive for most patients and impossible for the uninsured. This is an area where government subsidies can have a major positive impact. For a patient with a legitimate need, there is no reason to be denied life saving technology because they are unable to pay the price. Another major ethical hurdle involves testing. One cannot ethically test a mechanical heart on a healthy subject. Even if the subject gives full consent, it is widely accepted that it would be morally wrong to remove a healthy heart and implant an experimental mechanical replacement. Research using animals has limits with applicability to humans. The only individuals whom the potential benefits outweigh the experimental costs to life are those who are suffering from severe end-stage heart failure; the extremely ill. These people typically have a list of severe health problems and it becomes incredibly difficult to fully test the effectiveness of an experimental device. Further, nobody should look to mechanical organs as a substitute for maintaining a healthy, well-balanced lifestyle. While mechanical organs will be of great benefit to those born with genetic condition or who suffer the consequences of poor lifestyle, they are not a perfect substitute for the natural heart. Mechanical organs are the next best things to death. The healthy biological heart is backed by millions of years of evolution and performs incredibly well under a wide variety of environmental conditions. Families and individuals need to seriously think if “life at all costs” is really what they want. Is it really worth it to be kept alive if it means suffering on a daily basis. The quality of life is important. Eventually, as the technology improves and mechanical organs become a closer match to the biological organs, one can envision there will be people who choose to remove healthy organs and replace them with mechanical versions. This will open a floodgate of ethical concerns. Today we have athletes who inject themselves with steroids to artificially enhance performance. It is highly foreseeable that one-day athletes will request artificial organs and limbs. They can become the ultimate superhuman. While this is very far off and it might be difficult to find a qualified doctor willing to perform the operation, it is most certainly something to look out for in the coming decades. References
|







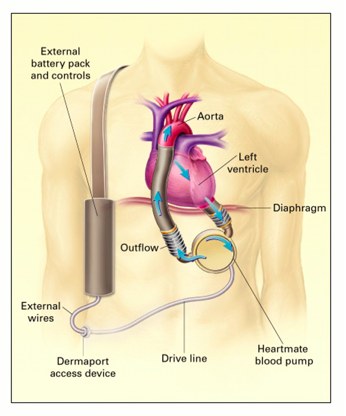 designed by Dr. Adrian Kantrowitz, boosts the native heart by taking up over 50% of its function (Mitka). The major advantage is that the patient can keep the natural heart, which can receive signals from the brain to increase and decrease the heart rate as needed. With the completely mechanical systems, the heart rate is fixed.
designed by Dr. Adrian Kantrowitz, boosts the native heart by taking up over 50% of its function (Mitka). The major advantage is that the patient can keep the natural heart, which can receive signals from the brain to increase and decrease the heart rate as needed. With the completely mechanical systems, the heart rate is fixed.